FAQs
What is Cancer
Breast Cancer
- Non-invasive breast cancer
- Invasive breast cancer

Frequently Asked Questions
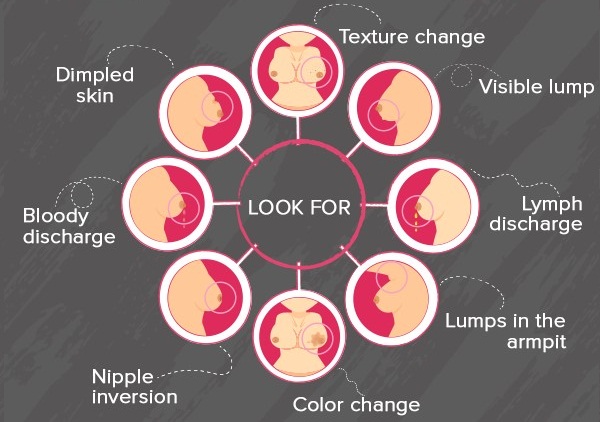
- Painless lump in the breast
- Blood stained nipple discharge
- Nipple retraction
- Any other changes in the breast which persist for more than two weeks
Regular physical activity can help prevent breast cancer.
Balanced DietEat a balanced diet rich in vegetables, fruits and proteins and low in fat
TalkTalk to your breast surgeon about mammogram if you are above 40 years.
Not all lumps are cancerous. In younger age, just before and during monthly periods, one can feel lump(s) in the breast(s). A breast lump can be any one of the non- cancerous conditions like a breast cyst, a fibro-adenoma, an abscess, a sebaceous cyst under the breast skin, etc. A lump which is firm or hard to feel and usually does not go away after periods is suspicious of cancer and needs urgent attention. It is advisable to consult your breast surgeon to get assessed clinically. Some tests may be advised to understand the nature of the lump. Some of the tests which may be needed are Mammography, Ultrasound scan of the breasts, MRI of breasts, FNAC (Fine needle aspiration cytology), Core needle biopsy, etc.
What to do if you have family history of breast cancer?There is a slightly high risk of developing breast cancer, if your first degree relative, i.e. mother, father, siblings etc. (male or female) has been diagnosed with breast or ovarian cancer. If more than one relative have been suffering from breast cancer or they have been diagnosed at a young age then the risk relatively increases. Nearly 5-10 % of breast cancers are due to inherited genetic abnormalities. A positive family history does not mean that one has to live in constant fear of developing the disease. Being aware of this fact is the most important thing. It is recommended that one should do regular self- breast examination once a month starting at the age of 18-20 years …..read more, get oneself examined by a breast surgeon if any change is noticed in the breast(s). The relatives (especially siblings and children) of patient who has been diagnosed with breast cancer at a young age (less than 40 years) should start screening 5 years before the age at which the patient was diagnosed. MRI of the breasts is usually recommended screening modality for those who are younger than 40 years. After 40 years of age annual mammography is recommended as a screening tool. This helps in diagnosis of breast cancer at an early stage.
What to do if you have nipple discharge?Many women notice nipple discharge at various stages of life. Majority of the times the discharge is due to benign (non- cancerous) conditions of the breast. The discharge can vary in colour from watery, light yellow, milky, yellowish green or brown, or reddish, blood stained. It can be present in one or both sides at the same time. Nipple discharge can be seen coming out from a single duct opening or from multiple duct openings on the surface of the nipple. Many a times the nipple discharge is seen only after pressing below the nipple. Some women continue to have milky white discharge several months after discontinuing breast feeding. Common causes of nipple discharge are fibrocystic breast disease, duct ectasia, intra-ductal papilloma, etc. If the discharge is spontaneous (i.e. seen without pressing behind the nipple) or is seen to be coming from a single duct opening every time and is blood stained, then you are advised to consult your breast surgeon immediately. In addition to clinical assessment, you may be advised to undergo certain tests like ultrasound scan with high frequency probe, mammography, cytological examination of the discharge, or sometimes MRI of breasts, etc.
